Suboxone
Suboxone is one of three medications approved for medication-assisted treatment (MAT) of opioid dependence. The other two are methadone and naltrexone. MAT combines approved drugs and supportive therapy, such as counseling.
Despite proven safety and lower costs, access to the drug was not satisfactory in the past. In 2012, 48 states and the District of Columbia had higher rates of opioid abuse than the capacity of buprenorphine treatment.
Over the last few years, access to buprenorphine treatment has increased significantly. In 2003, only 121 opioid treatment programs (OTPs) used buprenorphine. The number increased by over six-fold, to 779 in 2015.
Less than one in one hundred people at substance use facilities received buprenorphine in 2007. The proportion increased to eight in one hundred people in 2017. Now, the United States capable of treating 3.6 million people with buprenorphine.

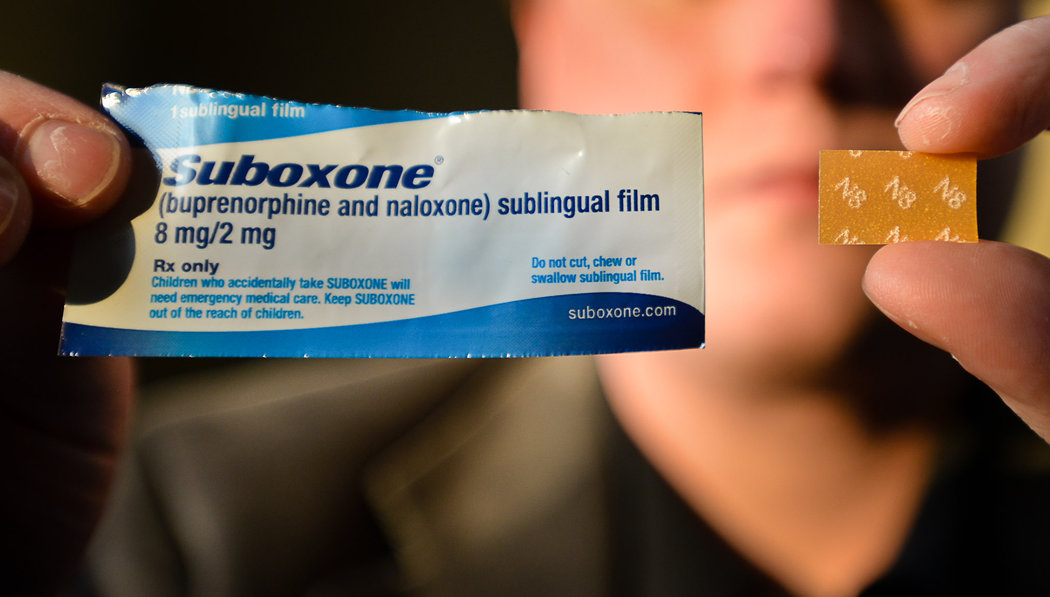
What is Suboxone?
Suboxone is the brand name of a medication used to treat opioid dependence. There are two different drugs in Suboxone and naloxone. The drug comes in the form of sublingual tablets and film. The United States Food and Drug Administration approved it to treat opioid addiction in 2002. The drug partially activates opioid receptors. As a painkiller, it is about 25 times more potent than morphine.
Naloxone prevents opioid drugs from attaching to the receptors in the brain. Naloxone, in Suboxone, is not active. However, it becomes active if the tablets are crushed (or film strips are dissolved) and the solution injected into the body. The active drug blocks the euphoric effects and causes discomfort. That way, naloxone helps reduce the misuse and abuse.
Suboxone helps:
•Withdraw from heroin and methadone
•Reduce opioid cravings
•Improve the quality of life
Apart from Suboxone, there are three brands of medications containing buprenorphine and naloxone.
They are:
• Zubsolv (Sublingual Tablet)
• Bunavail (Buccal Film)
• Cassipa (Sublingual Film)
What are the Differences Between Suboxone and Subutex?
Both Suboxone and Subutex contain buprenorphine, but Suboxone also contains naloxone. The brand Subutex is not available now. No brands containing only buprenorphine are used to treat opioid dependence. Instead, they are used to treat pain. In the street, each 8 milligram (mg) tablet is available for five to ten dollars, and 8 mg film can be acquired for about $15.
Street Names
Suboxone AKA
Buse
Strips
Big Whites
Stops
Saboxin
B
Sobos
Oranges
Small Whites
Sub
Bupe
Box or boxes
Is Suboxone Addictive?
Like all opioids, it can cause addiction and overdose. The addictive nature of a substance depends on three main factors:
•How fast they reach the brain (onset of action)
•The intensity of the euphoric effects (mild, moderate or strong)
•How long they act (duration of action)
A drug with rapid onset of action, strong effects, and short duration of action has the highest potential for addiction. For example, shooting (injecting) heroin produces quick, intense, and short-lived euphoric effects.
Unlike heroin and fentanyl, buprenorphine causes less euphoric effects that last longer. Thus, the risk of addiction is low but still warrants caution.
Drug Class
Buprenorphine is one of the members of a class of drugs called “mixed opioid agonist-antagonists.” Medicines in this class show varying activity on opioid receptors. The activity depends on the type of receptors they act on and the dose used.
Examples of other drugs in this class are:
•Pentazocine
•Nalbuphine
•Butorphanol
Drug Schedule
It is a Schedule III controlled substance. The DEA categorizes substances depending on their abuse potential and approved medical use.
Schedule III substances have lower abuse potential than heroin, fentanyl, methadone, and morphine. Abusing these drugs may cause moderate physical dependence. Notably, dependence caused by Schedule III drugs is most often psychological.
Is Suboxone Safe?
It’s a safer alternative to heroin, methadone, and fentanyl because it has a “ceiling effect” on breathing. It means after a specific dose, further dose increases do not increase the risk of fatal breathing problems. On the contrary, high doses of fentanyl can cause cessation of breathing.
Most studies have compared the safety of buprenorphine with methadone. The results suggest that buprenorphine:
•Has a lower risk of overdose. It’s six times safer than methadone
•Causes fewer incidences of heart rhythm problems or arrhythmias
While it may cause liver damage when used by those with hepatitis, extensive studies suggest that those who have hepatitis can tolerate it. A physician should be consulted, however, in this instance.
Is Buprenorphine Safe for Use During Pregnancy/Breastfeeding?
Use During Pregnancy
According to the 2017 American College of Obstetricians and Gynecologists guidelines,
“In pregnant women with opioid addiction, buprenorphine is a safer alternative to methadone.”
Babies born to mothers on buprenorphine have higher birth weight and fewer signs of withdrawal. Still, some doctors believe Suboxone may not be safe. They argue that it can trigger withdrawal in the fetus. Nonetheless, the amount that reaches the fetus is often too little to cause any harm. Pregnant women who have a liver disorder should avoid using this drug.
Use During Breastfeeding
Reports suggest that using it while breastfeeding is unlikely to harm the baby. In fact, doing so could probably help control withdrawal in the baby and reduce the duration of withdrawal therapy.
Physician’s guidance should always be sought in the administering of any medications for those who are pregnant or breastfeeding.
Proper Use
Proper use is essential to reducing the risk of overdose, abuse, and potentially fatal consequences. Below is a list of things to remember when using buprenorphine.
•Use the drug only as recommended.
•A physician’s guidance should be sought for those who are pregnant or nursing a child.
•Never take larger doses or more frequently than recommended.
•Always handle the drug with dry hands.
•Place the drug under the tongue and allow sufficient time to dissolve.
•Never chew or swallow the tablet or film.
•How is Suboxone Abused?
•It’s abused primarily to get high. Though “high” is nowhere near the “heroin high,” abuse is not uncommon.
Methods of abuse include:
•Injecting the solution prepared from crushed tablets
•Snorting crushed tablets
•Injecting the solution made by dissolving the film strips
Symptoms of Abuse
The physiological and psychological effects that can suggest abuse are:
•Frequent or unexplained nausea and vomiting
•Severe mood swings
•Muscle aches
•Fever
•Headaches
•Difficulty falling or staying asleep
SUBSTANCE ABUSE
How is Buprenorphine Used?
It’s use is driven by the burgeoning opioid epidemic and peaked in the last five years. In 2017, doctors wrote 14.6 million prescriptions, a 60% increase from 9.1 million in 2012. Notably, the number of prescriptions surged to 9.3 million during the last three months of 2018.
A doctor may prescribe it if they have:
- Completed a Drug Addiction Treatment Act (DATA 2000)-qualifying training course
- Registered at the Drug Enforcement Administration (DEA)
- A network of mental health professionals and substance abuse treatment programs
- Private clinics
- Office-based practices
- Substance abuse treatment facilities
Short-term Effects of Buprenorphine
•Headache
•Weakness
•Sleepiness
•Diarrhea or constipation
•Dizziness
•Rapid heartbeat
•Itchy skin
•Excessive sweating
•Nausea/vomiting
•Stomach ache
•Sleep problems
•Back pain
•Vision problems
•Constricted pupils
It can cause potentially fatal side effects in some instances, including severe allergic reactions, liver damage, and high levels of serotonin in the body.
Immediate medical attention is necessary if any of the following are evident:
•Hives and rashes
•Swollen tongue, lips, or throat
•Yellow skin
•Light-colored stools
•Restlessness
•Hallucinations (feeling things that are not there)
•Stiff muscles
•Breathing difficulties
•Slowed breathing
•Dark urine
•Goosebumps
•Fever
•Uncontrollable muscle twitching
•Lack of coordination
Long-term Effects of Buprenorphine
Doctors prescribe it for prolonged periods in people undergoing opioid maintenance therapy. Long-term use can cause the following side effects.
Hormonal imbalances
Hormonal imbalances, such as adrenal insufficiency. Those with adrenal insufficiency have low levels of adrenal hormones in their bodies. Examples of adrenal hormones include cortisol or stress hormone, epinephrine, and norepinephrine.
Liver damage
In some people, the drug may raise the levels of liver enzymes.
Abuse and dependence
Drug abuse refers to any use other than recommended. Dependence occurs when one cannot function normally without taking an addictive drug.
Can You Overdose on Suboxone?
Overdose risk is much less than the risk of methadone. Those with a history of opioid use may tolerate up to 32 mg of buprenorphine. Overdose deaths from buprenorphine alone are rare.
Mixing the drug with alcohol, benzodiazepines (BZDs), or other CNS depressants can be dangerous. Benzodiazepines are of most concern, as they are commonly used in opioid-dependent people. A doctor may prescribe a BZD to relieve sleep problems and anxiety during early treatment. One study found BZDs and alcohol in 82 percent and 58 percent of all cases of buprenorphine poisoning, respectively.
In 2016, buprenorphine toxicity caused five deaths. During the same year, US poison centers documented 2,160 cases involving only buprenorphine. Emergency department (ED) visits involving abuse/misuse of the drug increased by nearly five times from 4,440 in 2006 to 21,483 in 2011. Overdose can cause potentially life-threatening conditions. These include inflammation of the liver and kidney failure.
Symptoms of an Overdose
At the first suspicion of an overdose, a doctor should be contacted immediately, or consult the American Association of Poison Control Centers at 800-222-1222. If the symptoms are severe, calling 911 or visiting the nearest emergency room is an immediate and necessary recourse.
An overdose can present the following symptoms:
•Headache
•Diarrhea
•Anxiety
•Chills
•Dizziness
•Burning sensation in the tongue
•Coma
•Nausea and vomiting
•An upset stomach
•Excessive sweating
•Tiredness
•Decreased sensitivity to touch
•Breathing difficulties
•Death
Quitting Suboxone
One should never stop using Suboxone without a physician’s help and guidance. Abrupt discontinuation can cause many undesirable withdrawal symptoms. To reduce the severity of withdrawal, the doctor may recommend the reduction of the dose over several weeks. It is known as tapering. There are two methods of Suboxone taper. They are rapid taper (several days) and longer taper (at least a month). The doctor will decide which method will benefit each individual’s condition the most.
Withdrawal from Buprenorphine
Suboxone is used to ease withdrawal from opioids, including heroin. Sadly, the drug itself can cause withdrawal. The risk is high for those who are stopping the drug suddenly (cold turkey). On the bright side, withdrawal from Suboxone causes mild symptoms and is rarely severe.
The withdrawal symptoms appear about two days after the last dose. They last for about a month. The severity of the symptoms depends on the dosage taken and the duration of use.
During withdrawal, these may occur:
•Mild flu-like symptoms
•Muscle pain
•Joint pain
•Runny nose
•Watery eyes
•Headache
•Digestive problems such as nausea, vomiting, and stomach ache
•Increased irritability
•Anxiety
•Low moods
•Problems with focus
•Cravings
•Sleep problems
Most physical symptoms peak during the first three days of withdrawal. During this period, some are most likely to resume drug use. Many of the symptoms gradually subside over time. Cravings and low moods may persist after a month of withdrawal. Some people who have severe symptoms may need to take clonidine (Catapres). Nonetheless, the efficacy of clonidine in Suboxone withdrawal has not been widely accepted.
Using the following tips can help make symptoms more manageable.
•Eat a balanced diet.
•Exercise regularly.
•Get seven to nine hours of quality sleep each day.
•Sharing thoughts with trustworthy people.
Top Three Suboxone Myths
Using Suboxone Isn’t Safe, Because It Can Cause Overdose and Addiction
Truth: Buprenorphine (Suboxone) is perhaps the safest drug for treating opioid dependence. When used as prescribed, there is little risk of abuse or overdose. The drug is about six times safer than methadone in the general population. A long duration of action and mild euphoric effects make it one of the most suitable medications for treating opioid dependence. Since its approval in 2002, Suboxone has been involved in only a few cases of overdose deaths.
Suboxone Shouldn’t Be Used for Long Periods
Truth: Doctors prescribe the drug for short-term and long-term opioid treatment. While opinions may vary, no solid evidence supports that only short-term use of Suboxone is beneficial. In the long-term maintenance treatment, it can safely be used for a year, or even longer.
It Isn’t Advised to Switch to Suboxone from Methadone
Truth: Studies show that buprenorphine (Suboxone) is as effective as methadone. Thus, one can switch to Suboxone from methadone. Nonetheless, if there is a history of heavy opioid abuse, Suboxone may not provide the desired results. A physician should be consulted about drug options.
Treatment for Buprenorphine Addiction
As with other opioid addiction, the first stage of treatment is detox. Detox, under medical supervision, is a safe way to remove Suboxone from the system.
During detox, many withdrawal symptoms may occur, including cravings, mood swings, irritability, headache, muscle pain, and sleep problems.
Because Suboxone causes low physical dependence, most of these symptoms go away after a week. However, some psychological symptoms and cravings may persist for several months. The doctor may prescribe some drugs if symptoms are severe. Examples of the drugs include clonidine (Catapres) and naltrexone (Vivitrol).
After detox, other treatments may be needed to prevent relapse and maintain abstinence. Suboxone addiction is not usually severe. Thus, treatment at an inpatient rehabilitation facility may not be necessary.
Most people recover from outpatient treatment programs. These programs provide a structured environment where they will learn life skills and share their experience. Notably, these programs teach skills to help reintegration into the community.
An outpatient treatment facility also provides various forms of psychotherapy (talk therapy). Two types of psychotherapy have been routinely used in opioid addiction treatment. They are cognitive behavioral therapy (CBT) and contingency management (CM).
CBT
CBT is a short-term talk therapy. It is based on the theory that our thought patterns guide our drug use behavior. Thus, identifying and correcting problematic thought patterns can help treat addiction.
CM
CM is another effective non-drug therapy for opioid addiction. Contingency management is based on the theory that a person repeats those behaviors that are rewarded. Thus, CM focuses on rewarding a particular behavior with the intent of reinforcing that behavior. According to CM, abstinence is rewarded; chances are the patient will be more likely to abstain from drug use.
Resources
- Congressional Research Service. Buprenorphine and the Opioid Crisis: A Primer for Congress.
- Connecticut State Department of Consumer Protection. Buprenorphine and Naloxone Combination.
- BMJ Open. The relative risk of fatal poisoning by methadone or buprenorphine within the wider population of England and Wales.
- The American College of Obstetricians and Gynecologists. ACOG Committee Opinion. Opioid Use and Opioid Use Disorder in Pregnancy.
- Canadian Family Physician. Buprenorphine-naloxone uses in pregnancy for treatment of opioid dependence.
- Drug Enforcement Administration. BUPRENORPHINE.
- The Ochsner Journal. Suboxone: Rationale, Science, Misconceptions.
- Journal of Clinical Psychopharmacology. Interactions on mixing diazepam with methadone or buprenorphine in maintenance patients.
- European Journal of Clinical Pharmacology. Benzodiazepines and alcohol are associated with cases of fatal buprenorphine poisoning