CO-OCCURRING DISRODERS
OBSESSIVE-COMPULSIVE DISORDER
Obsessive-compulsive disorder (OCD) is more than just a person who washes their hands too much or repeatedly checks to see if the stove is off. A person with OCD has an obsessive need to repeat behaviors or experiences and often unpleasant thoughts.
In many people, OCD doesn’t appear just by itself. A person may also struggle with addiction as a means to try and escape the thoughts and behaviors that rule their lives. While no cure exists for OCD or substance abuse disorder, there are many treatment approaches a person can utilize to improve their daily functioning and overall health. This article will explore the connections between OCD and addiction, as well as how therapists approach their treatment.
A DEFINITION


What is OCD?
- Presence of obsessions, such as recurrent thoughts, urges, or impulses that a person tries to suppress or neutralize, often without success
- Presence of compulsions, such as repetitive behaviors (e.g. hand washing or checking something). These acts are usually aimed at trying to relieve anxiety or ward off bad events
- A person’s symptoms must not be related to the side effects of a medication or illegal substance
- A person’s symptoms are not due to another disorder, such as generalized anxiety disorder, body dysmorphic disorder, or major depressive disorder
A doctor may also classify a person’s disease severity if they recognize their symptoms are a problem. However, some people may not recognize their thoughts and beliefs regarding their disorder are false. An example could be “If I don’t lock the door 10 times before I leave, something bad will happen to me.”
What Causes OCD?
Doctors don’t know exactly what causes OCD. A theory is the disorder is the result of abnormal brain functioning that impacts the brain’s circuits. According to BeyondOCD, an OCD advocacy organization, a study of the brains of people with OCD found that those with OCD have 32 percent more inflammation in brain tissue than those who don’t. However, they have identified a few risk factors that make a person more likely to experience OCD. These include:
• Family History of OCD
• History of Physical or Sexual Trauma
• Being an Adolescent or Young Adult
Doctors have also identified a greater number of young people experience OCD symptoms after experiencing a streptococcal infection. They call this condition Pediatric Autoimmune Neuropsychiatric Disorder Associated with Streptococcal Infections, or PANDAS for short.
Postpartum OCD
In addition to OCD in the young population, doctors have identified another OCD syndrome known as postpartum OCD. An estimated two to three percent of new mothers experience this condition. Some of the symptoms doctors associate with postpartum OCD include:
- Excessively or frequently washing a baby’s clothing, bottles, or other items
- Isolating the baby and keeping family members away for fear they will harm or contaminate the baby
- Experiencing frequent thoughts or fears of harming the baby
Both postpartum OCD and postpartum depression can occur in a woman. These require treatments to help a person free themselves from obsessive thoughts and compulsive behaviors.
Signs of OCD
True to its name, doctors divide OCD and its symptoms into two separate categories: obsession and compulsion. Obsessions are usually thoughts or fears that a person cannot escape, even when they know they may be irrational. The symptoms are usually distressing to the person and can impair their abilities to function at work and school.
Obsessive Signs
- Fear of germs or that their food, water, or medication is poisonous
- Fear of losing an item or putting it in the wrong place
- Need to have objects in a symmetrical or particular order
- Having unwanted and repetitive thoughts of unpleasant things, such as death, violence, or sex
Compulsive Signs
Compulsions are behaviors a person routinely engages in, even when they know the behaviors are harmful to them.
• Cleaning one’s hands or other body parts over and over
• Hoarding behaviors, where a person refuses to throw away any belongings
• Frequently arranging and re-arranging particular items and becoming upset should those items get out of order
• Counting items over and over
Checking items repeatedly, such as constantly checking to ensure a door is locked
• Constantly requiring reassurance regarding behaviors or choices
OCD Statistics
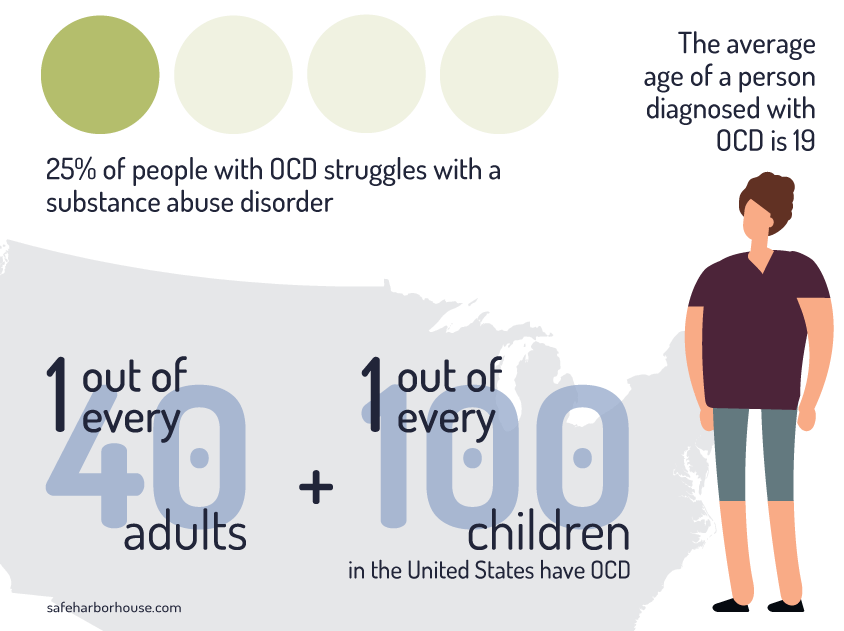
According to Beyond OCD, an estimated 1 in 40 adults and 1 in 100 children in the United States have OCD. The condition is responsible for a number of health complications and is in the top 20 causes of disability-related illness worldwide in ages 15 to 44 years old. The average age of a person diagnosed with OCD is 19. An article on the International OCD Foundation’s website estimated that the average occurrence of substance abuse disorders and OCD is about 25 percent. This means that about one in four people with OCD struggles with a substance abuse disorder.
OCD and Addiction: A Dual Diagnosis
Doctors know that OCD and substance use disorders, such as alcohol addiction or drug abuse, are common. However, they haven’t conducted a significant amount of research as to how many people with OCD struggle with addiction and vice-versa.
Rates of OCD and SUDs
A study of 323 participants published in the Journal of Anxiety Disorders found that 27 percent of patients with OCD also struggled with a substance use disorder (SUD). Of those who struggled with a substance abuse disorder and addiction, an estimated 70 percent reported they struggled with OCD for at least one year before struggling with addiction. The younger a person is diagnosed with OCD, the more likely they are to develop an alcohol use disorder.
The journal article also found 25 percent of those who seek medical treatment for OCD suffer from a substance abuse disorder. The most commonly abused substances among those with OCD were alcohol, cannabis, and cocaine.
Researchers also found that having OCD significantly impaired the abilities of a person to function in daily life. For example, those with OCD and a substance abuse disorder were more likely to receive disability benefits compared to those who did not have both disorders. Also, those who had both conditions were more likely to be house-bound, experience psychiatric hospitalizations, and report suicide attempts than a person who had one condition or the other.
Connection between OCD and SUDs
Doctors don’t know exactly why OCD and substance abuse disorders commonly occur together, but there are a few theories. The first is that a person with OCD may turn to substance abuse as a means to escape from their everyday struggles with OCD. For example, a person may drink alcohol in excess to escape their thoughts or to help them sleep so they can avoid the urge to engage in repetitive behaviors. Doctors may call these theories as self-medication or tension-reduction models. Doctors also know that people with OCD and substance abuse often have many emotions in common. These include fear, isolation, and shame.
A study published in the Journal of Anxiety Disorders also found that most people with OCD experienced their OCD symptoms before their substance abuse disorder. However, it is possible that a person with SUD may start to develop OCD following the development of their substance abuse problem.
Misconceptions About OCD
Many people are familiar with OCD on a surface level. For this reason, a person who likes things neat and clean may joke that they are OCD; however, this is not the same as the true diagnosed condition. As a result, misconceptions exist about what OCD is and what it isn’t. Correcting these misconceptions is an important step because it helps people to better understand what OCD is and to lessen the stigma of people who do suffer the condition.
PEOPLE WITH OCD ARE COLLECTORS
OCD is not a person who collects. Collectors may gather items, such as sports memorabilia, antiques, model cars, or coins. Collectors may be preoccupied with their collections and enjoy talking about them, but it isn’t OCD. Some people may also boast a wide body of knowledge about a particular topic, such as history or sports. While they may have a special and time-consuming interest in these topics, they don’t necessarily have OCD.
CELEBRITY “OBSESSIONS”
When people hear the word “obsessed,” they may also think about romantic relationships and intentions. For example, a person can be “obsessed” with a celebrity. They may have a crush on a person and read about them in magazines or have their posters on their walls. This doesn’t mean that a person has OCD. While there are people who are problematically obsessed with others and engage in behaviors like stalking, these people do not have OCD.PEOPLE WITH OCD TEND TO GAMBLE, LIE, OR SHOP
People with OCD do not typically engage in behaviors such as gambling, lying or shopping. A person with these behaviors may have an impulse control problem, but they don’t necessarily have OCD.
Study Results on OCD and Addiction
Treating OCD can be challenging and treating it with addiction at the same time can be further complicating. However, doctors have developed several approaches over the years that have helped a person gain control over their addiction as well as their obsessive thoughts.
A STUDY ON BEST PRACTICES
Although a significant body of research about substance abuse disorders and OCD doesn’t exist, there is some information about best practices for treatment. For example, a study published in the Journal of Substance Abuse Treatment studied 60 people diagnosed with OCD and substance abuse disorders. Researchers assigned participants into three different groups. One group received treatments that combined OCD and substance abuse treatments. Another received treatment for their substance abuse only. The third group received treatment for their substance abuse disorder and also participated in progressive muscle relaxation classes.
DUAL-DIAGNOSIS TREATMENT IS MOST SUCCESSFUL
At the study’s conclusion, authors found those who received treatment for OCD and substance abuse at the same time were more likely to stay in treatment. They also reported more significant reductions their OCD symptoms and their severity. When researchers followed up with participants after one year, those treated for OCD and substance abuse disorder were more likely to be sober.
Dual-Diagnosis Treatment Approaches
MEDICATIONS FOR OCD
Doctors often use a combination of therapeutic approaches to treat OCD and addiction. They may specifically prescribe medications to help reduce obsessive thoughts and symptoms. Examples include selective serotonin reuptake inhibitors (SSRIs). These medications may take anywhere from 10 to 12 weeks to reach their effect. Another medication called clomipramine is a serotonin reuptake inhibitor. Doctors prescribe this medication to treat OCD as well. Unfortunately, medication treatments alone aren’t usually enough to help a person treat their OCD. According to Beyond OCD, an estimated one in three people with OCD won’t respond to medication treatments alone.
MEDICATIONS FOR ADDICTION
Doctors may also prescribe medications to treat a person’s substance abuse disorder. These medications depend on the substance a person abuses. For example, the U.S. Food and Drug Administration (FDA) has approved medications to treat addiction to opiates and heroin. Examples of these include methadone and Suboxone. However, the FDA hasn’t approved treatments for some substances of abuse, such as methamphetamines.
The FDA has also approved some medications as deterrents to return to substance abuse. For example, a person can take medications if they struggle with alcohol that will make them feel very ill if they drink again.
Doctors may also prescribe supportive medications to treat withdrawal symptoms. Examples can include medications to control nausea or to reduce the risks that a person would experience seizures.
EFFECTIVE THERAPIES FOR OCD AND ADDICTION
In addition to medications, doctors also recommend therapeutic approaches for those who struggle with addiction and OCD. A common behavioral therapy approach is cognitive behavioral therapy (CBT). This approach involves identifying behaviors that lead to addiction or compulsive thoughts and teaching a person to change their thinking to more positive and effective options.
Doctors may use a specific CBT type called exposure and response prevention (EX/RP). This therapy involves exposing a person to their anxiety or fear in small doses and teaching a person how to better deal with the emotions they feel. This approach should only be employed by a medical professional.
12-STEP PROGRAM
An additional therapy approach is twelve-step facilitation. This includes participation in a 12-step substance abuse treatment. These program types include Alcoholics Anonymous or Narcotics Anonymous. These treatment plans include a structured approach with 12 steps to treat a person’s addiction. Participation in 12-step programs can be helpful for those with OCD because they are less socially isolating. A person also increases their social interactions in a positive way so that people focus on their recovery. However, 12-step programs shouldn’t be a substitute for cognitive-behavioral therapies and medication-assisted treatments.
BARRIERS TO DUAL-DIAGNOSIS TREATMENT
Ideally, a person can receive treatment for both disorders in one place. However, it isn’t uncommon that a person may seek treatment for OCD, yet a facility recommends they seek treatment for their substance abuse disorder and vice-versa. This can represent a challenge for a person in finding a facility to treat them. Some rehabilitation facilities may coordinate with a behavioral health facility to help a person receive care for both disorders.
SAFE HARBOR TREATMENT CENTER
Recovery is Possible
A significant number of those with OCD also struggle with substance abuse addiction. Often, the addiction is a means to self-medicate to treat their problem. However, substance abuse does not solve a person’s OCD problem; it only serves to worsen it over time. As a result, a person should seek treatment for OCD and substance abuse disorder. This is preferably accomplished at a rehabilitation facility that treats both conditions. Through a variety of approaches, including medication administration, individual therapy, and group programs, a person can start to manage both conditions and live a healthier lifestyle.
RESOURCES
- http://beyondocd.org/information-for-individuals/clinical-definition-of-ocd
- http://beyondocd.org/ocd-facts/what-is-ocd
- https://www.nimh.nih.gov/health/publications/obsessive-compulsive-disorder-when-unwanted-thoughts-take-over/index.shtml
- http://beyondocd.org/ocd-facts
- https://iocdf.org/expert-opinions/treating-co-occurring-ocd-and-substance-use-disorder-what-professionals-need-to-know/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2705178/
- http://beyondocd.org/ocd-facts/what-ocd-isnt
- https://www.sciencedirect.com/science/article/pii/074054729290032J

