WHY CAN’T I KEEP FOOD DOWN?
Rumination Syndrome:
If you’ve never heard of rumination syndrome, you wouldn’t be the only one. Rumination syndrome is still quite rare, and only recently has it gotten more attention on the medical field. If you are an avid Netflix watcher, you might have seen the show “Diagnosis” on which rumination syndrome was featured in episode five of the series.
What Happens?
It Makes You Spit Up Food
Rumination syndrome is a rare and chronic condition where people involuntarily spit up (regurgitate) their recently eaten food. The name rumination disorder comes from the word “ruminate,” which is what cows do when they chew undigested food. People may either re-chew and re-swallow the food or spit it out.
It is Not the Same as Vomiting
Unlike vomiting, the food that is spit back up has not been digested and tastes the same as when it was first eaten. While vomiting involves gagging, regurgitation is not forceful and is described as an effortless process of the food coming back from the stomach into the mouth through the esophagus (the tube that connects the throat to the stomach).
It is Like Burping
It is actually similar to burping, but rather than burping up gas; the reflex causes food to come back up the esophagus. This can occur minutes after eating or up to one to two hours after. For some people, regurgitation happens after every meal, and for others, it may happen less frequently, such as once a week.
A DEFINITION
Rumination Syndrome isn’t Voluntary
It is Involuntary
Many people mistake rumination syndrome for bulimia or other eating disorders; however, unlike eating disorders, rumination syndrome is involuntary, and the person is not intentionally spitting up their food.
Medical Classification
This places rumination syndrome in a category of disorders known as Functional Gastrointestinal Disorders. A functional disorder means that some type of bodily function is not working as it should, but because nothing is physically wrong, medical tests have a hard time detecting such disorders.
It isn’t Caused by a Physical Problem
Self-harm is a term used to describe the actions someone takes to intentionally injure themselves repeatedly. The self-harming activity is usually done on impulse and is not meant to cause death.
Self-harm is also commonly referred to as self-mutilation, self-abuse, self-injury, and engaging in self-injurious behavior (SIB). The medically correct term for self-harm is non-suicidal self-injury (NSSI).
WHO CAN GET RUMINATION SYNDROME?
Initially, it was believed that rumination syndrome occurred mainly in young children with developmental disabilities. Now, it is known that rumination syndrome can occur in both children and adults who have normal cognitive functions. In other words, rumination syndrome can occur in almost anyone and at any age. However, it is more common amongst people with developmental disabilities, anxiety, depression, or other psychiatric disorders.
Causes
Because rumination syndrome is rare and largely misunderstood, it is not entirely known what causes it. It is a functional disorder, meaning that physically there is nothing wrong with the body, so it can be extremely hard to detect and even harder to know what causes it.
Trigger Events
The medical histories of patients with rumination disorder show that symptoms often begin after some type of triggering or stressful event. This could be a viral infection, a disease, a traumatic event, physical injury, or other stress occurring in the person’s life. If someone had the stomach flu and were experiencing severe episodes of vomiting, the reflex might stay in place, and the abdominal muscles might continue to contract even after the illness goes away. In the Netflix show “Diagnosis,” the patient who had rumination syndrome had been bitten by a raccoon, which was believed to be the triggering event that caused rumination syndrome.
Illness
If the triggering event is some type of illness, the individual may develop sensitivity in the nerves of the digestive tract, which can make having food or liquid in the stomach uncomfortable. This can cause the body to adapt by contracting the abdominal muscles in an effort to regurgitate the food. This becomes a learned habit, meaning that even after the trigger/illness is gone, the habit and reflex of regurgitation might remain.
Still Unknown
In some cases, rumination syndrome does appear to occur at random, and there is no identifiable trigger or cause.
Is Rumination Syndrome Like Eating Disorders?
No. Rumination syndrome is often mistaken for bulimia (an eating disorder characterized by binge eating followed by vomiting) or anorexia (a refusal to eat in order to lose weight). Bulimia and anorexia are both emotional disorders where the person’s image of their own body is so distorted that they have an obsessive desire to lose weight through extreme means. Rumination syndrome, on the other hand, does not stem from body image issues or a desire to lose weight. Eating disorders are intentional, but rumination syndrome is unintentional. Bulimia involves the vomiting of digested food, which will be very acidic, but rumination syndrome does not involve vomiting but rather the spitting up of undigested food.
Risk Factors
Some risk factors that may increase the chance of getting rumination syndrome in both children and adults include:
- Having an acute illness
- Having a mental illness
- Experiencing a psychiatric disturbance
- Undergoing major surgery
- A stressful event/experience
Symptoms Of Rumination Syndrome
The main symptom of rumination syndrome is the regurgitation of food shortly after eating. In addition, these are other symptoms that you might experience if you have rumination syndrome:
- Food regurgitation
- Weight loss
- Bad breath
- Fatigue
- Dry mouth or lips
- Dehydration
- Feeling of fullness
- Nausea
- Decreased quality of life
- Stomach aches or indigestion
The symptoms of rumination syndrome are the same in both children and adults. In addition to uncomfortable physical symptoms, children, in particular, may also feel ashamed or embarrassed by their condition and may experience social problems. People with rumination syndrome might also have to miss work or school as a result.
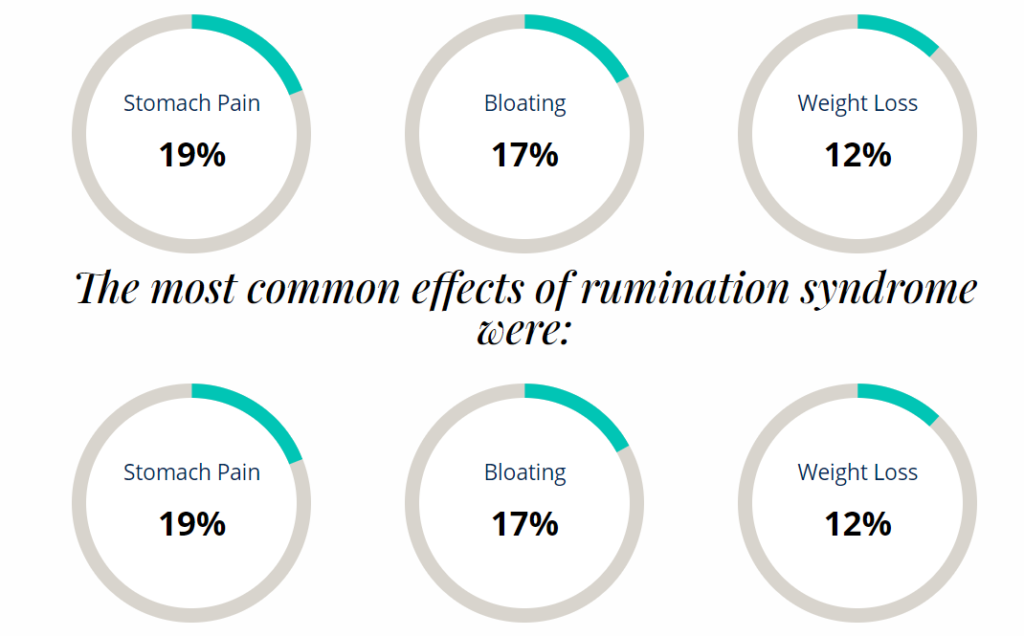
Health Effects
Aside from the uncomfortable symptoms that rumination syndrome presents, there are also various health effects that can occur if rumination syndrome goes untreated. Luckily, rumination syndrome does not have many severe physical health effects. However, some possible effects are:
- Excessive weight loss
- Severe abdominal pain, nausea, bloating
- Dental erosion
- Embarrassment
- Lowered school attendance
- Anxiety
- Stress
- Esophageal problems
- Malnutrition
- Bad breath
- Social isolation
- No longer participating in sports or athletic activities
- Depression
DIAGNOSIS
Because it is a functional disease and nothing is physically and visibly wrong with the body, rumination syndrome is very hard to diagnose. That is also one of the reasons why it is believed to be a rare syndrome: it is probably under-diagnosed. Rumination syndrome is also very often misdiagnosed as an eating disorder, as a vomiting disorder, as heartburn, or as gastroesophageal reflux disease.
Medical Criteria
While there is no formal diagnostic testing required to identify rumination syndrome, the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-V) lists the following diagnostic criteria for rumination disorder:
Repeated regurgitation of food for a period of at least one month. Regurgitated food may be re-chewed, re-swallowed, or spit out.
The repeated regurgitation is not due to any other medical condition (such as gastrointestinal disorder).
The regurgitation does not occur in relation to another eating disorder such as anorexia, bulimia, or bing-eating disorder.
When regurgitation occurs along with another mental disorder or developmental disorder, the symptoms are severe enough to require medical attention.
Additional Questions the Doctor Will Ask
In addition to these criteria, it is important that healthcare providers ask the correct questions and look into the patients’ medical history. Some questions that need to be asked are:
- How the food tastes when it has been spat up
- How soon after eating does the regurgitation occur
This is important as many patients mistake regurgitation for vomiting, but the difference is crucial in reaching a diagnosis.
It is also important to obtain a patient’s medical history to try and determine whether they had any type of prior illness or triggering event that could help explain the cause of the syndrome.
COULD YOU HAVE RUMINATION SYNDROME
If you suspect that you might have rumination syndrome, some questions that you can ask yourself, and that might help a doctor determine a diagnosis include:
- What does the regurgitated food look like and taste like?
- How long after you eat does regurgitation happen?
- Has regurgitation ever woken you up from sleep?
- Can you feel or hear that you are about to regurgitate or vomit?
- Have you ever taken medications to treat reflux? If so, do they help?
Additionally, while there are no official diagnostic tests that are used specifically to identify rumination syndrome, healthcare providers may perform blood tests and imaging in order to rule out other possible disorders or diseases and to evaluate levels of dehydration and malnutrition.
Typically, any type of diagnostic test such as a blood test should appear normal as rumination syndrome is a functional disorder, and physically, everything should be normal.
Rumination Syndrome Treatment
According to research, medications are not useful in treating rumination syndrome, although reflux reducers might help in the short term. Since rumination syndrome is a behavioral disorder, treatment for the condition involves behavioral modification and therapy. Currently, the behavioral therapy that is used to treat rumination syndrome involves teaching people special breathing techniques (diaphragmatic breathing) in order to control the urge to regurgitate — in other words, relearning how to eat and digest food correctly is an important first step in treatment.
Behavioral Therapy
Because regurgitation is thought to be a learned behavior that turns into an involuntary pattern, it is important to reverse that pattern of behavior. The way that this is done is by teaching new routines that compete with the urge to regurgitate and work to replace negative behaviors with better ones. These techniques are typically taught by behavioral psychologists.
Re-learning Eating Habits
Often times, patients will eat a meal while under the guidance of a behavioral psychologist in order to re-learn habits surrounding food. In addition to breathing techniques, this might also involve changes in posture while eating, removing distractions during meal times, reducing stress, and biofeedback (a technique used to learn to control some of your body’s functions).
Breathing Techniques
Breathing techniques are easy to learn and have proven to be very effective. For most people, the symptoms will vastly improve or disappear altogether. Early treatment is recommended in order to minimize the health risks and social effects that can occur from untreated rumination syndrome.
Important Aspects to Treating Rumination Syndrome
To provide you with a straightforward list, the National Eating Disorder Association has compiled a list of important aspects of rumination syndrome treatment.
Education
It is very important that patients and their families understand the diagnosis, so they do not worry that it is another condition or disease. Families who participate in treatment see the best results.
Treat the trigger symptoms
Symptoms such as nausea or bloating that occur after eating should be treated to try to reduce the frequency of regurgitation.
Undo the habit
Treatment should include learning about how habits are formed, learning about what your abdominal muscles are doing, learning new behaviors for the abdominal muscles, and maintaining relaxation during meals.
Re-train the stomach to hold food again
Patients should start with small amounts of food and gradually increase the stomach’s ability to tolerate larger amounts of food and liquid.
Teaching self-regulation
Patients should learn how to regulate the autonomic nervous system to allow for more relaxation and the management of trigger symptoms.
Identifying and addressing other problems
Some patients with rumination syndrome also struggle with depression, anxiety, worry, and stress. These problems often occur as a result of having rumination syndrome but can also be part of the trigger. Struggling with these problems makes treating rumination syndrome more difficult, so it is important to implement a treatment plan that targets any co-occurring problems or disorders.
How Common is Rumination Syndrome?
Now that you’ve learned what rumination syndrome is, you might be wondering how common it really is. Because rumination syndrome is quite rare, experts have a hard time determining how many people are truly impacted by it, but it is clear that rates of rumination syndrome are increasing. This could be because doctors are more aware of the syndrome, so they are more likely to diagnose it, but could also be because cases of the syndrome really are increasing.
Sri Lankan Study
While there haven’t been any large-scale studies done to determine the rates of rumination syndrome, there was one study conducted in Sri Lanka that surveyed over 2,000 children between the ages of 10-16.2 The study found that:
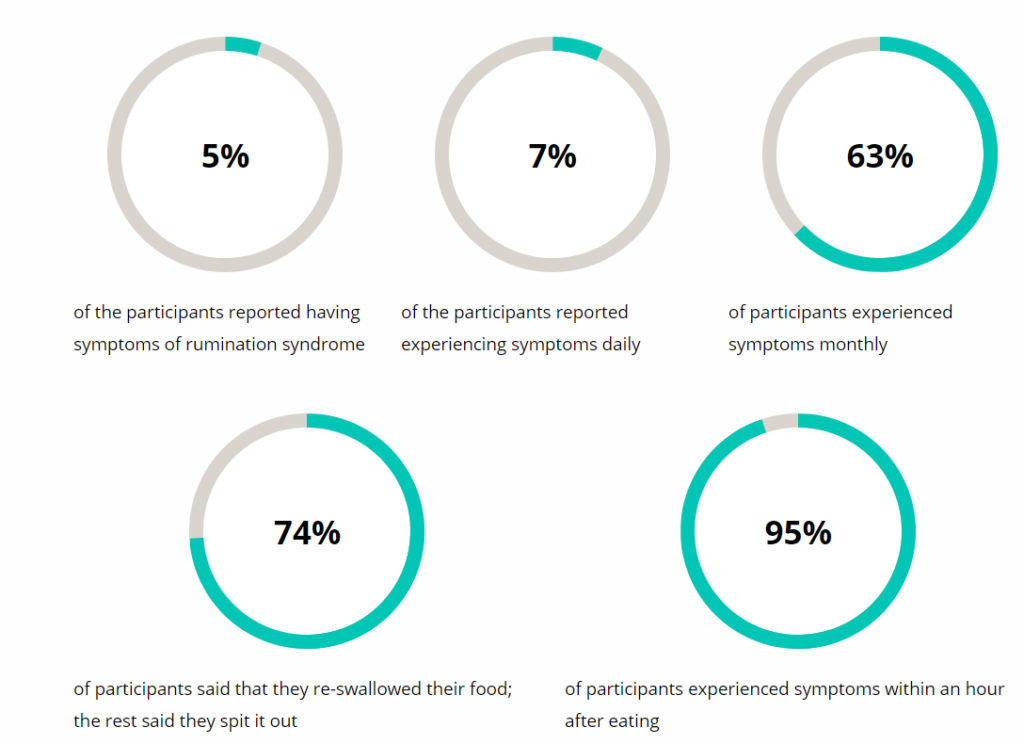
The rates of rumination syndrome were fairly similar amongst females and males. However, rumination syndrome peaked at age 14 for males and at age 16 for females.(3)
What About in Adults?
Rates of rumination syndrome in adults are largely unknown, partly due to the fact that rumination was thought to occur mainly in children. Amongst institutionalized populations, it is believed that between 6%-10% of people with intellectual disabilities have rumination syndrome. (4)

